Recent research shows that when we experience traumatic events, it increases physical health issues. What we see, feel, and experience has a direct impact on our minds and our bodies which means trauma and health are very connected. In this article, we take a closer look at how your past traumas and health are connected.
What is Trauma?

Trauma is the emotional response resulting from incomprehensible experiences. Suffering an attack, surviving an accident, or experiencing a natural disaster isn't something everyone goes through. It's not normal to face these types of experiences. When we do, our brains and bodies remain impacted.
Three Types of Trauma
Trauma isn't limited to a one-off event or accident. There are three main types of trauma.
- Acute – This type of trauma comes from a single incident that is often out of the blue and not typical for the environment. It can include witnessing a trauma, experiencing a trauma, or surviving an accident or illness.
- Chronic – Trauma is repeated over time and includes issues like domestic violence, homelessness, and other prolonged exposure to dysfunction.
- Complex – Represents someone exposed to a variety of traumas including multiple traumatic experiences as well as prolonged traumas combined.
Making the Connection Between Trauma and Health
Your Body Keeps Score
Author Bessel Van Der Kolk, MD published the popular book The Body Keeps the Score illustrating how trauma impacts the body and causes a wide variety of mental and physical problems.
If you battle with your mood or struggle with staying positive – Click here now for “nature's happy”.
Our bodies are designed to withstand trauma. When we face a traumatic experience, our brains are especially hardwired to kick into gear. Our brains secrete hormones and send signals to our nervous system that help us act in the face of threats and keep us safe.
But the imprint of the experience on our mind can cause immediate and long-term issues, including:
- Post-Traumatic Stress Disorder
- Anxiety and other mental health disorders
- Digestive issues and autoimmune diseases
- Increased risk for stroke or heart attack
The Impact Trauma Has on Your Body

Sometimes a traumatic situation will immediately trigger a response in your body.
Witnessing a tragedy or experiencing something traumatic can cause an upset stomach, headache, or any number of other symptoms.
Other times, your body may protect itself at the moment and seem to disregard what's happened only to react later on when you may not make the connection.
Either way, your body is keenly aware of what's going on and has a conscious or subconscious reaction.
People living with chronic or complex trauma may have normalized the sensations in their bodies and have no awareness of the connection between their illnesses, disease, or poor health and trauma.
Connecting the Dots
If you haven't given much thought to your health and how it may be impacted by trauma, it's time to connect the dots.
Taking a look at your personal history and comparing it with your medical history can be eye-opening.
Once you recognize a potential connection between your health and any traumas you may have experienced (or are experiencing) you can begin to take a holistic approach to your healing.
If you battle with your mood or struggle with staying positive – Click here now for “nature's happy”.
Digestive Issues May Be Linked to Your Trauma
Have you ever been scared, worried, or looked back on something in the past and started to feel queasy or worse, have to head for the bathroom? It's amazing how our bodies can be triggered by our thoughts, isn't it? Research shows that four out of ten people suffer from some sort of gastrointestinal issues including everything from lactose intolerance to IBS.
Your Digestive Issues May Be Cause by What You Are Eating
Everyone experiences digestive issues from time to time. Eating the wrong thing can cause momentary distress and for some, allergies can cause chronic illnesses that must be managed for a lifetime. Some of the common digestive disorders include:
- Gastroesophageal reflux or GERD
- Chronic Diarrhea
- Chronic Constipation
- Gastroenteritis
- Ulcers
Over 73,000 people seek help from their doctor every year to manage these and other digestive issues. For many, changing their diet can reduce or eliminate the symptoms or presence of certain diseases, but what happens when diet changes don't help?
Your Digestive Issues May NOT be Caused By What You're Eating
People who have suffered, or are living with trauma, often experience the same digestive issues, but their diet isn't the culprit. That's because some physical issues aren't the result of a medical condition. They may be caused by tension in the body. Most often the gut.
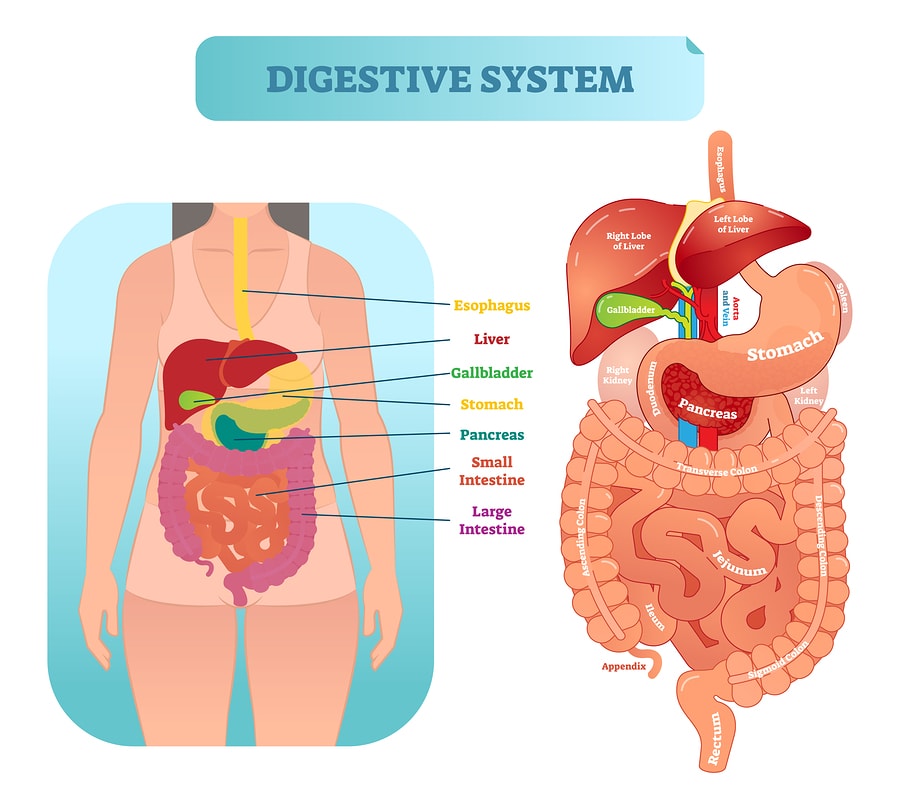
Our gut and our brain are connected. The gut includes the mouth, esophagus, stomach, and intestines. When we are nervous, upset, or experiencing stress, our digestive system is often triggered by the brain and begins to experience dis-ease. This can be as mild as feeling sick to our stomach or intense as cramping. Over time, it can also lead to a host of digestive illnesses.
How You Can Improve Your Irritable Digestive System
If you have no medical reason for digestive issues it may mean your body is reacting to trauma. The good news is there are many things you can do within your control that tame your digestive system.
Try these suggestions:
Use Your Breath
Breathing is a powerful way to regulate your mind and body. You can help relax your mind and nervous system and allow your body to settle through deep, conscious breathing. You can accomplish this by closing your eyes for a few minutes, meditating, or practicing moving meditation by taking a walk.
Change the Scenery
One of the easiest ways to disrupt nervousness is to change the scenery. If you are inside, get outside. Or if you are in the car, stop and take a brisk walk.
Breaking up the scenery can help distract the mind and the body's reaction to traumatic thoughts.
Choose Foods Wisely
Even if there is no medical explanation for your digestive issues, what you eat still matters. Choosing healthy foods that promote gut health is an extra layer of protection against pain and upset. Eat a fiber-rich diet with plenty of hydrating fruits and vegetables for a stable gut.
Digestion issues are incredibly common and it's possible you are suffering because of what you eat, or it could be what's eating you. Recognizing the role trauma plays in our bodies can help reduce many digestive issues you may have thought were medical.
Chronic Pain May Have a Psychological Origin
Traumatic experiences leave their mark on the mind and the body. Experiencing trauma, whether it's one time, or repeatedly, changes how the brain reacts to stress. Our bodies produce hormones that help deal with temporary stress. Over-production of these hormones can keep the body in a state of hyper-vigilance that results in aches and pains throughout your body.
Some, but not all include:
- Muscle and joint pain
- Digestive pain
- Chronic headaches
Studies linking chronic pain and trauma indicate that it's possible that our bodies can react to single and repeated incidents of trauma long after the acuity or safety issues are gone. That means your current aches and pains may be rooted in past trauma.
Childhood Trauma and Chronic Pain
The ACE, or Adverse Childhood Experiences, study was a partnership between the Centers for Disease Control and Keiser Permanente hospital to determine whether abuse, neglect, and loss during childhood could indicate risk factors for mental and physical illness in adulthood.
The study identified categories of abuse, neglect, and loss and determined that the higher the number of traumatic experiences, the higher the likelihood of illness down the line. Data reveals an alarmingly high correlation between childhood trauma and a host of diseases, addictions, and illnesses including chronic pain.
Post-Traumatic Stress and Chronic Pain
Many people think of veterans when they hear the term post-traumatic stress disorder, also known as PTSD. But military personnel are not the only ones who experience this disorder. PTSD occurs in people who have difficulty recovering from traumatic, terrifying, or life-threatening events.
PTSD affects all races, genders, and age groups. PTSD can lead to chronic issues including nightmares, intrusive thoughts or memories, isolating behaviors, depression, and much more. Chronic pain is often associated with PTSD resulting from tension, overproduction of stress hormones, and other factors.
Your Pain May Be In Your Head
Over 50 million people per year live with chronic pain. Most of them seek relief from their medical provider who is focused on their bodies. As a matter of fact, being told pain is all in your head is considered an insult, but it's likely true. More and more doctors are looking beyond the possible physical triggers for pain and including the psychological origins too. If you have experienced trauma, even if it was a long ago, you may be reacting physically to something psychological.
Reporting Past Trauma to Your Doctor
An ounce of prevention is worth a pound of cure. The old adage encourages each of us to take action whenever possible to prevent illness, injury, or disease. Its timeless advice that can keep us safe and healthy. Routine checkups help our medical providers get a baseline of our health, including our physical and mental history, so they can monitor your care over time.
Don't Wait to Be Asked about Trauma
Now more than ever, providers are tuning into mental health issues that present as physical illness. We've all completed paperwork reporting our health history including what illnesses, injuries, or familial histories might affect our health. Be sure to include any traumatic experiences in your history.
Don't be afraid to share trauma history with your physician, even if they don't include it in their intake. Knowing about traumatic experiences you've dealt with can help them offer you preventative care as well as make better decisions about current treatments.
Some key trauma's worth reporting include:
- Accidents or acute illnesses
- Abuse or neglect
- Domestic violence
- Victimizations
- Significant losses
- Familial histories of alcohol or drug abuse
Any of these or other traumas can help your doctor better understand what influences could be affecting your overall health.
Discuss Coping Skills With Your Doctor
Everyone deals with stress in their own way. Coping skills are conscious and subconscious strategies people use to manage difficult things. What causes trauma for one person may not affect another in the same way. Similarly, what one person does to cope, may look nothing like what someone else does.
Reporting your typical coping skills to your physician can help them identify dangerous coping skills or connect the dots between your health and the coping skills you may engage in. For instance, drugs, alcohol, or food are often used as coping skills for trauma. This means addictions and obesit may be connected to trauma and require a specific type of support.
Take a Team Approach to Your Health Care
Having a primary care physician is common, but you may need more providers on your team. If you've experienced trauma of any kind, singularly or repeated, you may benefit from including a psychologist or psychiatrist on your care team.
Your history greatly impacts your health. Be confident and feel safe sharing your past with your primary care provider, even if you see yourself as a survivor and moved on. The truth is, what happened may affect your health and you deserve to be the healthiest version of yourself possible. Help your health care provider connect the dots by giving them a full account of your physical and mental history.
Signs Your Body May be Reacting to Trauma
Whether you are aware of it or not, you may be reacting to trauma in a physical way. If you are currently living with trauma you may be well aware of the aches, pains, physical and emotional discomfort triggered by trauma.
Some signs include:
- Disrupted sleep
- Irritable stomach
- Changes in eating
- Anxious thoughts
CBD Sleep Tincture – Free shipping nationwide!
Your Body Is Talking To You
Much of what we feel in our bodies is feedback. Pain is an indicator that something is wrong and needs to be addressed. It's part of our body's warning system helping us pay closer attention to what's going on. Sometimes we are in tune with our bodies and sometimes we aren't. When we take action, we generally find relief. If not, pain – both physical and emotional, can become chronic and we are not the better.
Signs Your Body Is Trying to Deal With Trauma and What Steps to Take
You've Gained or Lost Weight Quickly
Our eating is often disrupted as a traumatic response. From eating too little or too much, we may be coping with trauma through our diet. Left unchecked this can lead to eating disorders including obesity, anorexia, binging and purging, and more.
If you recognize that you are experiencing significant changes in your eating (or have a long history of disrupted eating) it's a clue you may need support. Consult your doctor and share your trauma history so they can help.
If you are sleeping too much (hypersomnia) you may be experiencing depression or having another reaction to trauma. Little to no sleep (insomnia) may also be triggered by anxiety, intrusive thoughts, and more.
Meditation apps like Zen12, structured bedtime rituals, and cutting caffeine prior to bed can be of great help. Your doctor may also have options available but needs to know bout any trauma that could be influencing your sleep.
Listen to your body and pay close attention to what it's sharing. Subtle or acute changes may be an indication you are reacting to trauma. From sleeplessness following an accident or acute illness to life-long food actions, your body is offering you clues that you may need to help cope and overcome trauma.



